Doctor Eddy Becquet
Foot surgeon
Hallux valgus Nice
Hallux Valgus Nice
Foot Surgeon
Doctor Becquet
Saint-George Clinic
Hall 3 - 3rd floor
2 avenue de rimiez
06100 Nice
Tel : 04 93 169 169
Percutaneous and minimally invasive surgery for the treatment of Hallux Valgus:

Locoregional anesthesia
Only one anesthetized limb
Operation in less than 30 minutes
Incision of 2mm to 2 cm
At home the same day
Complete patient autonomy
No rehabilitation
Immediate return to walking
Hallux Valgus Nice
Management of foot surgery
Hallux Valgus treatment in 4 steps
STEP 1
OUTPATIENT ADMISSION
Percutaneous and minimally invasive surgery allows for outpatient management.
STEP 2
ANESTHESIA
LOOREGIONALE
Popliteal block or ankle block (where only the foot is asleep)
STEP 3
THE SURGICAL INTERVENTION
Takes about 30 minutes with percutaneous and minimally invasive surgery.
STEP 4
SAME DAY RELEASE
After a passage in the recovery room, exit with the analgesic device.
Hallux Valgus Nice

Hallux Valgus Marseille
Definition of Hallux Valgus
Dr Becquet's office
The Saint George Clinic
2 Avenue de Rimiez
06105 Nice
Tel : 04 93 169 169
Hallux Valgus Nice
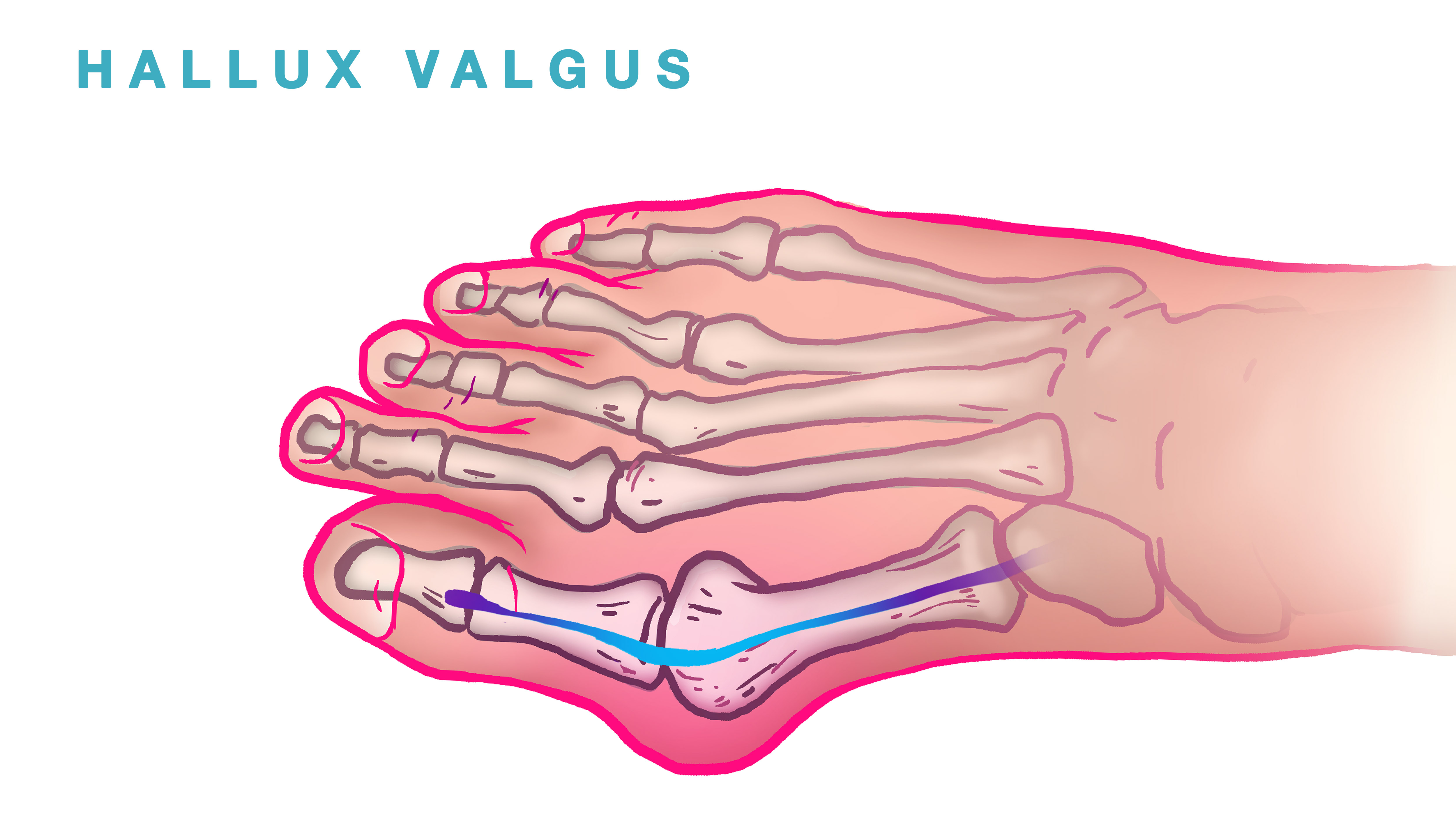
What is hallux valgus?
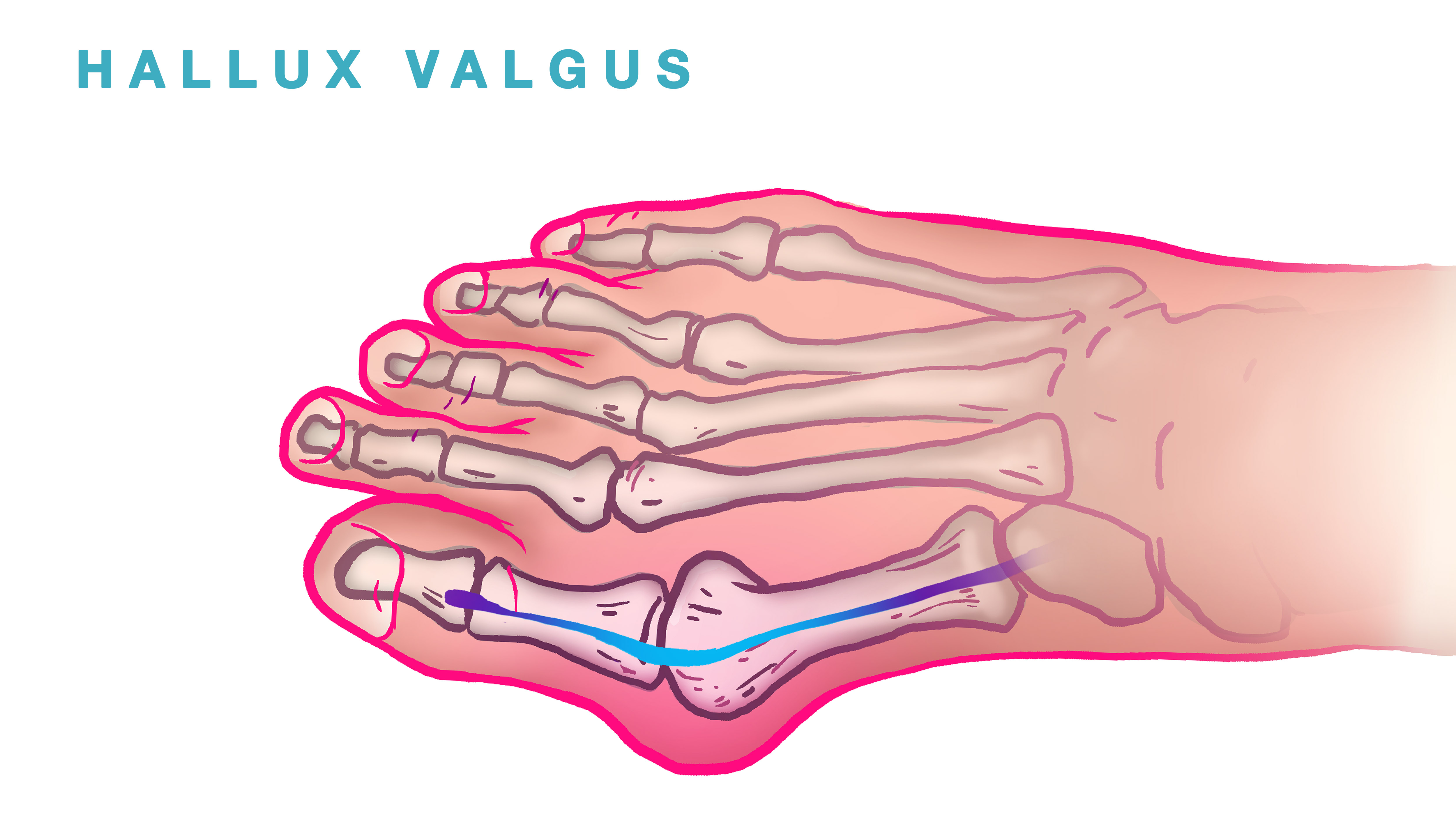
Under its complicated and learned name, hallux valgus is nothing more nor less than an extremely common ailment better known under the nickname of "bunion". It consists of a deformation of the big toe. The bump corresponding to the head of the bone (the metatarsal) grows, becomes inflamed and painful.
Normal locomotion is hampered and aggravates the pain, causing a vicious circle. Wearing shoes becomes particularly painful. This disease can be associated with arthrosis of the affected joint called hallux rigidus. In this case, both ailments must be treated.
Hallux Valgus Nice
Causes of hallux valgus
-This condition affects the female sex in more than 90 % of cases, most often around the age of 50, an age when hormonal impregnation changes due to the menopause: this would lead to hyperlaxity favoring the deformation of the big toe.
-In 30 % of cases, a family factor is found.
- Excess weight also favors the formation of hallux valgus.
-The morphotype of the foot is a key element that can explain the deformity of the big toe. Indeed, in 75 % of cases, hallux valgus is associated with an Egyptian morphotype corresponding to the case where the big toe is longer than the second toe.
With this morphology, the big toe is too long to be able to position itself normally in the shoe, in particular when it has a pointed toe: it is thus forced to deform itself by taking in width the place that it cannot take in length, hence the deformation in hallux valgus.
Conversely, the square foot (big toe the same length as the second toe) and the Greek foot (big toe shorter than the second toe) are much less likely to cause hallux valgus.
Moreover, one of the objectives of the surgery will be to obtain one of these two morphotypes when the pre-operative morphotype is Egyptian. In this way, the operation will eliminate a cause of recurrence.
-Hyperlaxity is not the only cause of the predominance of hallux valgus in women, since it is also caused by wearing shoes with pointed toes and/or high heels.

The treatment
To provide immediate relief, open-toed shoes are recommended, or alternatively, soft, flat shoes.
Painkillers may also be prescribed in some cases.
A podiatrist can also help to counteract the deformity of the toes with orthoplastics. This is only possible at the very beginning of the deformity, as this technique is not effective on a deformity that has already been fixed.
Moreover, wearing orthopedic insoles can be relevant when the toes are already clawed and the joints are already in a pronounced inflammatory state. This allows to reduce the pressure on these joints and thus to reduce this type of pain.
These treatments are symptomatic and will not prevent the long-term deterioration of the patient's foot. The only effective solution is surgery.
How to treat hallux valgus?
If the so-called symptomatic treatments do not succeed in stopping the evolution of the deformities and pain, only surgery can truly cure hallux valgus.
The choice of technique is made with the practitioner. There are minimally invasive techniques, with incisions of a maximum of 2 centimeters, and percutaneous techniques, which involve making very small incisions, of the order of a millimeter.
The procedure is performed under local anesthesia. Sedation can be offered to the patient if desired. The patient can leave the hospital the same day.
Spontaneous evolution of hallux valgus
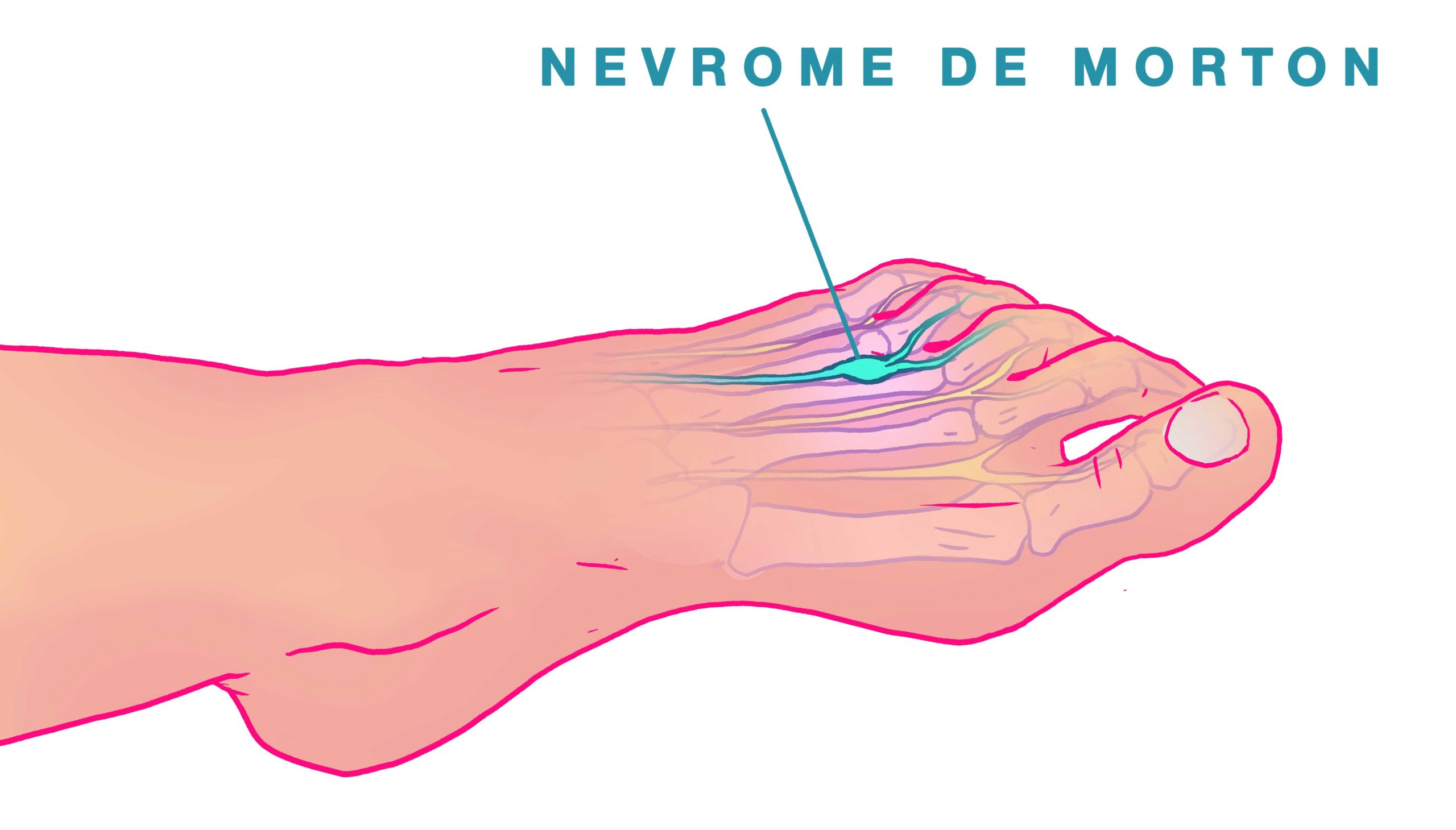
At the beginning of the evolution, the deformity of the big toe is isolated: the main reason for consultation remains the pain located opposite the exostosis, where one finds most often an inflammatory bursitis which can ulcerate and lead to an infection. In addition to the classic deformity, there may be a rotation disorder: the toe turns on itself, so that the nail no longer looks towards the zenith.
The deformity continues to evolve on its own, so much so that the hallux valgus ends up deviating the other toes laterally. This is how the 2nd ray syndrome appears, corresponding to the appearance of a claw on the 2nd toe pushed by the big toe which takes its place.
This deformity, initially limited to the 2nd toe, progressively extends to the entire forefoot.
The lateral toes retracted in the form of claws will come into conflict with the shoe, resulting in painful dorsal corns.
At the same time, under the effect of the claw, the metatarsophalangeal joint will subluxate or even dislocate, giving rise to metatarsalgia (pain when pressing on the metatarsal head).
It is always preferable to correct deformities when they are limited to the big toe, which simplifies the surgical procedure but also the postoperative course and reduces the recurrence rate.
What are the objectives of surgical treatment?
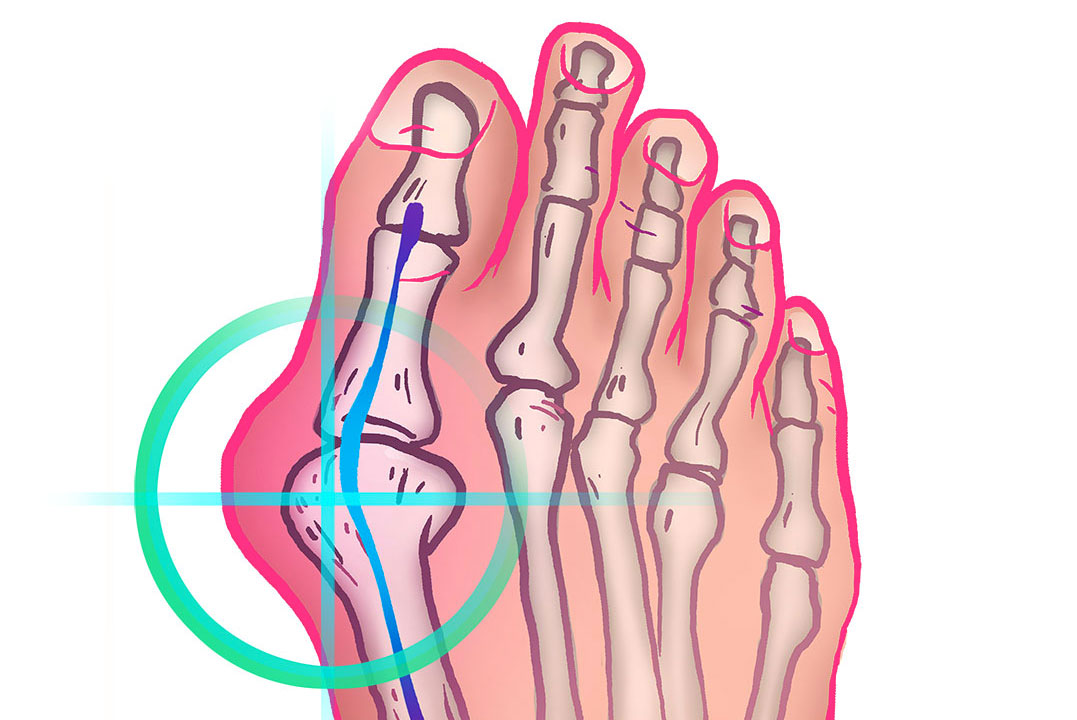
To reduce the deformity of the big toe, it will be necessary to reduce the excessive gap between the 1st and 2nd metatarsals (reduction of the metatarsus varus). To do this, a Scarf osteotomy is performed, allowing the translation of the 1st metatarsal towards the 2nd metatarsal.
The second bone procedure will be performed in the 1st phalanx by an osteotomy, allowing to achieve three objectives:
- reduction of the phalangeal valgus (= deviation of the 1st phalanx) by cutting a wedge-shaped segment of bone
- a shortening of the 1st phalanx allowing, in the case of an Egyptian foot, which could be a source of postoperative recurrence if not corrected, to transform it into a square or Greek foot.
- a correction of a possible rotation disorder in the big toe, in order to obtain a nail looking towards the zenith in post-operation.
To be successful, this surgical treatment must be accompanied by a rigorous postoperative protocol, both for the resumption of support and for the treatment of edema and pain.
Surgical techniques.
The minimally invasive and percutaneous techniques mentioned above are interesting, but more difficult to implement for the practitioner.
-Percutaneous surgery
This technique is only 15 years old in Europe. It is not specific to the treatment of hallux valgus nor is it systematic. As its name indicates, it is performed through the skin, with miniature burs introduced after making very small incisions with mini scalpels. The surgeon cannot directly visualize the operation. He has of course several tools to do so:
The first is fluoroscopy. It consists of using a very low-powered X-ray machine in order to make the exposure of the patient and especially of the surgeon completely acceptable. Of course, this technique only allows the visualization of bones. It is mainly a means of control for an experienced surgeon who can thus see the operated areas.
The second is the use by the surgeon of his touch and feel. The counterpart is that only very experienced surgeons can use the percutaneous intervention technique.
Obviously, when properly performed, it has only advantages. It is minimally invasive and allows a quick recovery after the operation.
-Minimally invasive surgery
This technique only requires incisions of less than 2 centimeters. However, the rest of the operation is comparable to "classic" surgery, with some percutaneous entries. The mini-chevron osteotomy, for example, is a recently developed technique that greatly minimizes the size of the operating field.

When to consult?
Consultation is highly recommended when the pain is embarrassing or even disabling when walking or putting on shoes. The pain may be more intense on the other toes, when they curl up into claws, than on the big toe itself, if the disease is already advanced.
It is therefore necessary to explain to the patient that the cure can only come from the treatment of the big toe, even if it is the other toes that may cause him more pain at the time of diagnosis.
Some people, especially young women, also consult for aesthetic reasons. Surgery to treat hallux valgus is then totally contraindicated.

What are the criteria for surgery?
The intensity of the pain is the main criterion. However, one should not wait until the pain becomes unbearable, as the operation may become more cumbersome with time.
It is indeed easier to intervene on an early hallux valgus than on the same disease that has evolved to the point of deforming all or part of the other toes.
This is all the more relevant as considerable progress has been made in recent years, particularly with regard to the invasiveness of the procedures, which minimizes the postoperative sequelae.

What are the advantages of these techniques for the treatment of hallux valgus?
The main advantages of these techniques are their minimally invasive nature.
-Pain is considerably reduced, as well as postoperative swelling and bruising.
-The resumption of support is immediately possible
-Outpatient care
-Faster recovery after surgery
Hallux valgus Nice
Foot surgeon
at the Saint George clinic in Nice
Doctor
Eddy Becquet


His method
Who is Dr. Becquet?
For more than 15 years, Doctor Becquet has been passionate about hallux valgus surgery. Aware that the traditional techniques for operating on this pathology resulted in long and painful after-effects, he quickly became interested in mini-invasive and percutaneous techniques that allow the surgeon to work with small incisions: the traumatic impact is much less on the operated hallux valgus and thus allows for a rapid recovery, both in terms of resumption of weight-bearing, which is immediate, as well as in terms of pain, which becomes non-existent or very bearable.
Hallux Valgus Nice
In order to obtain an even faster recovery after hallux valgus surgery, Dr. Becquet, always in search of innovation, has become an adept of Fast-Track. This is a method of patient management that aims to take the necessary measures to control postoperative stress in order to allow for a faster recovery and significantly reduce the risk of complications. Thus, in the context of hallux valgus surgery, Dr. Becquet and his team have set up a FAST-TRACK type of management combining :
Detailed oral and written information given to the patient throughout his care, thus contributing to his safety and making him master and actor of his care
Minimally invasive and percutaneous surgery is much less traumatic on the tissues thanks to the miniaturization of the incisions
Loco-regional anesthesia, which on the one hand facilitated outpatient treatment and on the other optimized pain control by a very gradual awakening of the operated foot
Outpatient hospitalization, by reducing the patient's stay in the clinic to a few hours, significantly reduces the anxiety-inducing nature of hospitalization. Indeed, the patient prefers to return quickly to his usual environment.
The personalized follow-up at home is reassuring for the patient. It will therefore promote rapid recovery after surgery:
- by the intervention of a service provider and his team of liberal nurses who will relay between the patient and the surgeon
- Daily visits to the patient's home thanks to a Smartphone application
- provider coordinator available 24 hours a day in case of problems
- daily report to the surgeon on the postoperative evolution of his patient
- oral and written information given to the patient on his surgical follow-up; the information given by the provider and his team of nurses is strictly identical to that given by the surgeon to avoid any discrepancy in the discourse which is a source of anxiety for the patient
- installation and follow-up of an analgesic diffuser to optimize the management of postoperative pain, which is already well controlled by the combination of mini-invasive and percutaneous techniques and local-regional anesthesia
Hallux Valgus Nice
CURRICULUM VITAE
Former intern of the hospitals of Lille 1997
Former chief of clinic of the hospitals of Lille 2002
Appointed Specialist in Hand and Foot Surgery 2002
Inter-university diploma in surgical pathology of the hand 2002
University Diploma in Vascular and Nerve Microsurgery 2000
University Diploma in Legal Compensation for Personal Injury 2004
Inter-university diploma in arthroscopy 2002
Lecturer for the National Diploma of Orthopaedic and Traumatological Surgery 2003
Lecturer in Anatomy of the Hand and Foot 2002
Associate member of the French Society of Hand Surgery
Member of the French Association of Foot Surgery
Hallux Valgus Nice
Cabinet
Find your orthopedist on the 3rd floor of Hall 3 and don't forget your health insurance card!




Hallux Valgus Nice
Foot surgery | Hallux Valgus | Nice
Dr Becquet's office
The Saint George Clinic
2 Avenue de Rimiez
06105 Nice
Tel : 04 93 169 169
Hallux Valgus Nice
Minimally invasive and percutaneous surgery
Outpatient procedure
Immediate resumption of support
An operation taking half an hour.
The operation can be performed by percutaneous surgery (incision of the order of a millimeter) or minimally invasive (incision of the order of a centimeter)

Hallux Valgus Nice
When is it necessary to have surgery?
The essential criterion is the level of pain that the patient complains of. For a similar deformity, the feeling of pain can be completely different from one person to another. When walking and shoeing become painful, it is essential to put the option of surgery on the table.
A hallux valgus cannot resolve itself, it will necessarily deteriorate more or less quickly and progressively evolve towards a self-deformation.
The earlier the surgery is performed, the more likely it is to permanently prevent recurrence and the less invasive it will be.
Indeed, the new techniques of intervention can be used, they are much less cumbersome and have postoperative consequences in general limited.
Percutaneous surgery
This technique appeared a few years ago and is increasingly used for hallux valgus. When properly performed, it offers many advantages. It consists of operating through the skin, making mini incisions just sufficient to pass miniaturized instruments.
It is not possible for the surgeon to see directly what he is doing. His touch and his experience will be essential. Nevertheless, he has a complementary technique that allows him to have a vision of the operation: the fluoroscopic image intensifier.
It consists of using a very low-powered x-ray machine that allows visualization of a key element in the treatment of hallux valgus: the bones. The device is of course qualified and sterilized, and its radiation level is low enough for surgeons to use it very regularly without risk. Note that this technique is only an aid and an extension of the surgeon's feeling. Nothing can replace his know-how and experience.
The advantages of this technique are obvious: the incisions are very small, pain is reduced and recovery is faster. It allows to avoid hospitalization.
What will be the level of pain?
The techniques used in the past have tarnished the image of this type of surgery to treat hallux valgus. Mini-invasive techniques and advances in local anesthesia allow for operations with very little pain in the overwhelming majority of cases.
As sensitivity to pain is not the same for all people, it is not possible to guarantee a "zero pain" procedure. However, the fact that this procedure is only performed on an outpatient basis is a sign that the management of postoperative pain does not generally pose any serious problems.
The management of pain is done very seriously in spite of everything. The quality of the local anesthesia will of course make it possible to feel no pain during the operation, but its effects will last at least 12 hours, limiting the pain that would immediately follow the operation. It is in fact in these hours following the operation that the pain can reappear, and the fact of having a prolonged analgesia in the operated area makes it possible to reduce post-operation stress and anxiety.
This device is complemented by a special device that will help the patient manage any pain once they leave the hospital. In the past, the patient had to stay in the clinic with an infusion to get an electric syringe.
Now the patient has a single-use analgesic diffuser which, with the help of home nurses, allows the patient to return home as soon as possible. This has several important advantages. The patient can indeed
- Eat at home and sleep outside the clinic
- To be quiet compared to the noisy environment of a clinic
- Be surrounded by your loved ones without restriction.
Operations to treat hallux valgus
When symptomatic treatment options are exhausted, the only option left is surgery. It is the only way to eradicate the cause and the pain. The technique to be used must be shared between the patient and the practitioner. There are several approaches. The first is the percutaneous technique, which leaves only almost invisible incisions, and the second is called mini-invasive, and will be performed with incisions limited to 2 centimeters.
The procedures are performed with local anesthesia and sedation (optional). The patient does not need to stay at the clinic in the evening, and can leave immediately after the procedure.
The mini-invasive technique
Surgery is said to be minimally invasive when the incisions made are of the order of 2 centimeters. However, the techniques used inside the foot are similar to those used in conventional surgery.
Once the incisions have been made, the surgeon will carry out the operation. By performing osteotomies with specific instruments, most of which are inspired by the percutaneous technique.

How long will it take for me to walk normally?
The techniques used allow the patient to regain support on his or her foot immediately after the operation, with the help of a specific shoe that the patient will have to keep for about a week. The resumption of support must be done with the entire sole of the foot. Indeed, one should not walk by pressing on the side of the foot or on the heel. This is not necessarily obvious and many patients instinctively do not respect this instruction. It is normal to be apprehensive about resuming walking after the operation, so a progressive protocol is recommended to reassure patients.
During the first week, walking is allowed but must be limited to what is strictly necessary. It is recommended not to leave your home. Treading and prolonged standing without walking should be avoided. When the patient sits or lies down, it is recommended to elevate the foot and leg.
The following week, the patient can walk outside the home, gradually. Walking periods should be limited to about 15 minutes, but should not exceed a total of two hours per day.
Gradually increase the amount of walking according to how you feel. It is advisable to abandon the special shoe for good and to put on a soft, flat shoe such as sneakers.
The time off work depends on the activity. Work can be resumed after two weeks in favorable cases. Of course, the activity must not require a lot of walking or repetitive "stomping". If this is not the case, the recovery period will have to be extended. In case of an early return to work, it must be possible to elevate the foot when the patient is sitting.
In general, as a precaution, the prescribed time off work is about three weeks.
New techniques for hallux valgus
For several years, much less invasive techniques have been developed to treat hallux valgus. They consist in making very small incisions instead of having a large operating field. They are therefore more complicated for the surgeon to implement.
The benefits of minimally invasive and percutaneous procedures for the treatment of hallux valgus
The percutaneous technique is very recent in Europe. It is a tool that must be adapted to the procedure. It is not systematically used for hallux valgus and should not be. It consists of performing an operation through the skin, using miniaturized instruments dedicated to this type of surgery.
This allows:
-The fact that the patient does not remain hospitalized
-Prompt recovery
-Less swelling and pain
-A possibility to walk very quickly after the operation.

How to manage dressings?
One week after the operation, the first dressing will be redone by the surgeon. The following ones will be done by a nurse. The liberal nurses are perfectly qualified to carry out these new dressings. They will be changed every two days for two weeks.
After two weeks, the threads will be removed by the nurse and you can then take a shower and wet the whole of the operated foot - drying the foot (possibly using a hair dryer) is important to avoid any maceration of the scar (presence of crusts when the scar is still recent). If externalized pins have been placed, your scar can also be wet, provided that the visible end of the pin is dried well.
Hallux Valgus Nice
Recovery from surgery:
a rapid phase
THE MODALITIES OF A RETURN HOME
Hallux Valgus Nice
Supervised by health professionals, specialists in percutaneous surgery in the Nice area
Hallux Valgus Nice
Successful return home is essential
This is an essential condition for recovery and success, and it is important to support it. A close follow-up is then deployed through the interventions of a dedicated team of nurses or private nurses. They will act as intermediaries between the surgeon and the patient on a daily basis:
Available at any time of the day or night
Presence several times a day at home.
Daily feedback to the surgeon on the patient's progress
Rigorous note-taking of the postoperative follow-up and written and oral communication of the surgeon's instructions and information.
Provision of an analgesic diffuser for good management of possible postoperative pain

Hallux Valgus Nice
Pain management after surgery:
When the patient leaves the hospital or clinic, he or she is given a specific device that allows for the gradual diffusion of painkillers through the intravenous route. This allows the analgesic effect of the anesthesia to be completed over time. The analgesics used are not derived from morphine, to avoid intolerance. This device is a progress in the sense that thanks to its miniaturization, the patient is not obliged to remain lying down, contrary to the traditional infusions. This device facilitates the patient's convalescence and reassures him. The liberal nurses who will follow the patient on his return are perfectly trained in its use.
This allows the patient to:
-Staying at home at night, and avoiding the noise and anxiety of the hospital environment
-Being surrounded by loved ones right after the operation, which reassures him and facilitates his recovery.

Management of postoperative edema
Pain management cannot be fully effective if instructions for limiting foot swelling are not followed. Swelling will distend the tissue and cause pain.
To prevent this, the following habits should be put in place as soon as the operation is completed:
1) Elevate the operated limb as soon as the patient sits or lies down. In fact, venous return is favored, which will help limit the edema.
2) Follow the protocol for resuming locomotion within three weeks after the operation. Failure to follow this protocol may lead to a resurgence of edema and therefore pain. As a reminder, here are the main points of this protocol:
Foot support should be limited to the strict minimum during the first week, and the patient should remain at home. Standing without walking or stomping should be avoided.
During the second week, the patient can go out of the house, limiting the walking time to periods of about fifteen minutes, not more than two hours per day. The postoperative shoe can then be removed permanently in favor of soft shoes, such as "Basket".
During the third week, the patient gradually increases his walking time according to his feeling.
3) Self-education which will consist of
-Quickly return to a flat footed stance after the operation
-Put on soft shoes after one week
-Resume walking after one week away from home
4) Icing, which consists of applying a cold pack when the patient's foot is elevated in a sitting or lying position. This will limit swelling and inflammation and therefore the onset of pain.

Zoom on the analgesic diffuser
It is a single-use material consisting of a mini-tank and a tube allowing the diffusion of the product.
Through a strong network of trained nurses, the reservoir is filled once a day and the patient's pain level is reviewed.
This diffuser is an important progress in the management of pain and allows the patient to go home, reassured, and as soon as possible.
When the device is removed, conventional oral painkillers are prescribed for about four days. After this period, painkillers must be taken according to the patient's feelings.
The three provisions aimed at limiting pain (local anaesthesia, portable diffuser and traditional oral treatment) follow a philosophy that aims to avoid the onset of pain and to maintain a good level of comfort for the patient.
The use of Fast Track, or rapid recovery after surgery.
Fast-track is a protocol created 20 years ago in Denmark. It aims to restore the patient's autonomy as quickly as possible after an operation, by taking multifactorial responsibility for his recovery. It covers measures taken during the operation and in postoperative management, as well as pain relief devices.
What is the purpose of fast-track?
The objective is to limit the psychological and physical stress related to an operation. This allows for a better recovery and increases the chances of success. It also allows to limit the risks linked to prolonged hospitalizations (nosocomial diseases, circulatory disorders etc.)
What is its use in the treatment of hallus valgus?
-The use of minimally invasive surgical techniques such as percutaneous and mini-invasive techniques. They are much less aggressive for tissues such as skin, tendons or muscles and therefore allow a good recovery.
-The use of a loco-regional anaesthesia which implies a limited sedation to the strict necessary. This avoids the need for general anesthesia, which can be a source of complications. Loco-regional anesthesia also allows a good level of postoperative analgesia to be maintained for several hours;
-The hospitalization in day hospital that these new techniques allow and the progress in anesthesia. The patient can quickly return to his normal routine, which reduces his stress and anxiety. This obviously contributes to a better recovery in the best conditions.
A close follow-up at the patient's home with a team of providers. They provide daily monitoring and a reinforced link with the care team and the surgeon. This makes it possible to secure the crucial weeks following the operation.
-Reinforced coordination between the perioperative staff and the hospital teams. This allows for a permanent follow-up of the patients. The messages given to the patient are perfectly coherent, which aims to reassure them.
-The patient does not just undergo the procedure. He is an actor and participates in his complete recovery. The patient is put in a situation to manage his own pain, thanks to a scale used with the help of the liberal nurses.
-Finally, it should be remembered that the level of information provided to the patient on the complete course of his or her care is essential to ensure that the care is perfectly mastered and that the complementary measures to be implemented after the operation are well followed.
To contact the
Foot surgeon | Hallux valgus Nice
Saint-George Polyclinic
Hall 3 - 3rd floor
2 avenue de rimiez
06105 Nice
Phone
04 93 169 169